Walking boots cause more problems than most patients expect. These medical devices, prescribed routinely for ankle injuries, trigger new pain patterns in 67% of patients – a startling statistic that deserves attention.
Your body responds to wearing a walking boot in ways that might catch you off guard. The numbers paint a concerning picture: 84% of patients develop fresh pain points within their first fortnight of wear. These typically surface in the lower back, opposite hip and knee. More troubling still, one-third of patients battle persistent pain at these secondary sites even three months after discarding their boot.
Medical professionals have long relied on walking boots to immobilise injured ankles. Yet recent evidence raises important questions about their wider impact on patient wellbeing. Blood clots from restricted movement, challenges with driving, and disrupted daily activities represent just a few potential complications. Understanding these effects proves vital for anyone facing weeks or months in a walking boot. Let’s examine what wearing one means for your body and daily life.
Physical Pain & Discomfort
Pain patterns tell a concerning story when it comes to walking boots. Studies reveal nearly 70% of patients develop new or worsened pain away from their original injury site. These secondary pain points create a ripple effect of discomfort throughout your body.
Where Does It Hurt Most?
Your lower back bears the brunt of walking boot discomfort. Next in line? The opposite hip and the knee on your boot-wearing side. The culprit behind this pain pattern lies in your boot’s thick sole. This extra height throws your body off balance, whilst the boot’s protective design forces you to walk unevenly.
How Long Will the Pain Last?
Boot-related pain follows a predictable timeline. Most patients (84%) notice new pain areas within two weeks of starting boot wear. When it’s time to remove the boot, 67% report secondary pain different from their initial condition. The most worrying aspect? One-third of patients still battle these additional pain points three months after boot removal.
What Helps with Boot Discomfort?
Try these proven strategies to ease your daily discomfort:
- Match your boot height with a raised shoe on your good foot
- Keep your steps shorter to fight the boot’s rocking motion
- Watch your alignment – the second toe should point where your knee faces
- Don’t hesitate to use a crutch or cane for persistent limping
Rest plays a vital role in pain management. Prop your leg above heart level to combat swelling. For quick relief, ice packs work well – apply them for 10-20 minutes every 1-2 hours in the first three days. Your healthcare provider might allow you to loosen your bootstraps during rest periods, helping blood flow more freely.
People with existing chronic pain face higher risks of developing secondary pain sites. That’s why regular chats with your healthcare provider about pain levels matter – they’ll help adjust your treatment plan as needed.
Risk of Blood Clots (DVT)
Blood clots pose a serious risk when wearing a walking boot. The medical term for this condition, deep vein thrombosis (DVT), demands careful attention throughout your recovery period.
Understanding DVT Formation
Your leg’s natural movement helps blood flow properly through deep veins. Walking boots restrict this movement, causing blood to move sluggishly. This slow circulation, paired with keeping your leg in one position, creates perfect conditions for clots to form.
Several factors multiply your DVT risk:
- Age beyond 50 years
- Current hormone therapy
- Previous blood clot history
- Excess body weight
- Heart disease or cancer
- Tobacco use
- Recent hospitalisation
Recognising DVT Symptoms
Your body sends clear signals when blood clots develop. Monitor your booted leg for:
- Unusual swelling compared to your other leg
- Tenderness or pain, particularly during movement
- Noticeably warm skin
- Unusual redness or colour changes
- Hard or thickened vein areas
Protective Measures
Smart prevention starts with movement. Within your doctor’s guidelines, try these proven strategies:
Regular movement matters most. Wiggle your toes and move your ankle gently three times daily. Ten seconds per session provides meaningful benefits.
Water intake plays a vital role in preventing clots. Keep well-hydrated unless your doctor advises otherwise.
Long car journeys? Stop every hour or two for movement breaks. Some patients need blood-thinning medicines based on their risk factors.
Emergency Warning Signs
Call emergency services immediately for:
- Unexpected breathlessness
- Breathing-related chest pain
- Blood in your cough
- Severe leg pain with swelling
DVT demands a swift medical response. Left untreated, clots can travel to your lungs, causing a life-threatening pulmonary embolism. Quick action significantly improves your chances of successful treatment.
Gait and Posture Changes
Walking boots change how you move. The controlled ankle movement (CAM) walker boot doesn’t just protect your injury – it reshapes your entire walking pattern. Most boots feature a rocker bottom design that forces significant changes in your walking mechanics.
What Happens to Your Walk?
Your body must create new movement patterns when wearing a boot. The rocker bottom design disrupts your natural walking rhythm. Your ankle and foot lose their normal range of motion, which reduces the sensory feedback your brain receives. This leads your body to develop compensatory movements, using muscles earlier and longer than usual.
Walking slows down naturally. The boot causes:
- Wider hip and knee movements during leg swing
- Changes in how you balance
- Different weight distribution
- Limited ankle movement
How Does Your Spine React?
One leg becomes effectively longer than the other, triggering a chain of postural adjustments. Even a small difference of 15mm can noticeably alter your pelvis position and spine alignment.
Your body responds with:
- Pelvis dropping on the shorter leg side
- Less hip socket coverage on the longer leg
- Gradual spine curvature changes
- Overall posture shifts
Which Joints Face Extra Stress?
Your body’s adaptations whilst wearing a boot place unusual demands on your joints. The hip on your longer leg turns inward, reducing its weight-bearing area. Meanwhile, the knee on that same leg bends more, increasing pressure on its outer surface.
The foot on your shorter side rolls outward, shifting your heel position and flattening your arch. These changes create abnormal forces throughout your leg.
Research shows three main areas face the most strain:
- Lower back (taking the heaviest toll)
- Hip opposite to the boot
- Knee on the boot side
These effects worsen the longer you wear the boot. Though a heel lift on your other shoe helps, it cannot fully correct these walking pattern changes.
Skin and Tissue Problems
Skin problems rank among the most troublesome complications of walking boots. From simple skin irritation to dangerous pressure ulcers, these issues demand careful attention throughout your recovery period.
Pressure Sores and Hot Spots
Pressure ulcers form when boots press constantly against your skin. Bony areas and boot edges face the highest risk. These aren’t mere inconveniences – untreated pressure points can lead to serious tissue breakdown.
Diabetic patients and those with limited mobility face heightened risks. The worst cases expose underlying tendons, sometimes requiring surgery. Watch for hot spots – reddened, warm areas that signal early pressure damage.
Managing Skin Irritation
Daily skin checks save trouble later, especially for diabetic patients. Look out for:
- Boot-related redness or warmth
- Burning or stinging feelings
- Toe numbness or tingling
- Boot-edge swelling
- Localised persistent pain
Moisture control matters enormously – trapped sweat quickly leads to skin problems. Never apply treatments without medical approval, as some products might harm healing tissue.
Protecting Your Skin
Success starts with proper boot fitting. The boot should feel snug but never restrict blood flow. Essential protection includes:
Long socks create a vital barrier between skin and boot. Swelling patterns change throughout the day, so strap adjustments help maintain comfort. Moving your leg every couple of hours prevents prolonged pressure.
For irritated areas, moleskin or Spenco’s Second Skin offers targeted relief. Steer clear of oils and lotions near the boot – they can damage materials and worsen skin problems.
Red flags demanding immediate medical attention include lasting redness, pain, or open sores. These signs might indicate serious tissue damage needing swift treatment.
Muscle Weakness and Atrophy
Muscles waste away surprisingly quickly in a walking boot. The numbers tell a stark story: calf muscles shrink by 21.9% and thigh muscles by 24.1% within weeks of wear.
What Happens to Your Muscles?
Your boot keeps you safe but at a cost to your muscles. Think of muscles like a machine – without regular use, they begin to power down. The boot’s protective nature creates an unfortunate trade-off: whilst healing your injury, it forces surrounding muscles into hibernation.
Science shows muscle changes start alarmingly fast – often within the first week of wearing your boot. The effects ripple through:
- Your calf muscles (triceps surae)
- Thigh muscles (quadriceps)
- Hamstring group
- Small foot muscles
Will Your Strength Return?
Recovery takes patience. Two months after boot removal, muscles still show significant weakness. Daily growth proves frustratingly slow – just 0.26% for calf muscles and 0.41% for thigh muscles.
Here’s the silver lining: hamstring muscles bounce back better, losing only 6.5% volume and recovering faster than other muscle groups. This finding shapes how physiotherapists approach rehabilitation.
Keeping Your Muscles Active
Medical professionals recommend specific exercises during boot wear. Try these muscle-preserving activities:
- Gentle non-weight exercises:
- Light calf tensing
- Hourly toe movements
- Hip and thigh contractions
- Upper body maintenance
- Core strength work:
- Chair-based exercises
- Adapted planking
- Safe leg raises
- Alternative activities:
- Pool exercises (doctor-approved)
- Upper body focus
- Heart-healthy options without foot pressure
Starting early makes all the difference. Just 30 minutes of gentle stretching daily helps prevent muscle shortening. Even small movements significantly slow muscle loss.
Follow your healthcare provider’s guidance on proper form and exercise intensity. A physiotherapist’s expertise ensures safe, effective movement. Remember – keeping unaffected joints mobile helps reduce swelling whilst maintaining strength and blood flow.
Sleep and Comfort Issues
Sleep quality suffers when wearing a walking boot. Night after night, patients struggle with disrupted rest, especially during their first few weeks of boot wear.
Night-time Troubles
Walking boots turn bedtime into a challenge. Their rigid frame, substantial weight, and bulky design make finding comfort feel impossible. Heat builds up inside the boot, leading to sweating and discomfort. Many patients toss and turn, managing only one to two hours of uninterrupted sleep.
Finding Your Sleep Sweet Spot
Your sleeping position makes all the difference in boot comfort. Back sleepers need pillows beneath their leg, keeping it above heart level. Sleeping on your side? Tuck a body pillow between your legs to support the boot and keep your spine aligned.
Best positions for peaceful sleep:
- Flat on your back, boot supported by three pillows
- Side-lying (good leg down) with body pillow support
- Half-sitting position to ease boot pressure
Making Nights More Bearable
Most doctors recommend keeping your boot on at night for the initial weeks. Simple adjustments help make this easier. Slightly looser straps before bed improve comfort without sacrificing support. Just ensure the boot stays secure enough to prevent unwanted movement.
Shield your bedding by wrapping the boot in a soft cloth or pillowcase. This clever trick both protects your sheets and adds cushioning comfort. Some patients dedicate an old pillow solely for boot protection.
Cool temperatures prove crucial for comfortable sleep. Walking boots retain heat, so keep your bedroom well-ventilated. When comfort remains elusive despite these measures, speak with your healthcare provider about possible solutions.
Essential night-time strategies:
Boot Management:
- Regular cleaning fights odours
- Create airflow opportunities
- Evening strap checks
Bedroom Setup:
- Cool air circulation
- Strategic pillow placement
- Proper leg elevation
Your specific recovery needs guide sleep requirements with the boot. Always follow your healthcare provider’s night-time wear instructions. Though some patients receive clearance to remove the boot after initial healing, never make this decision without medical approval.
Mental Health Impact
Your mental wellbeing matters just as much as physical healing when wearing a walking boot. Research highlights the psychological toll of sudden mobility changes, particularly the loss of independence many patients face.
How Does Limited Movement Affect Your Mind?
Missing your regular exercise routine triggers noticeable mood changes. Patients report feeling more irritable, experiencing unpredictable emotions, and battling higher stress levels. Poor sleep often follows, creating a difficult cycle that impacts emotional health.
Common psychological challenges include:
- Recovery timeline worries
- Daily task frustrations
- Pulling away from social activities
- Disrupted sleep patterns
- Changed eating behaviours
Regular exercisers often struggle most with these changes. Their usual stress-relief outlet disappears, leaving both mood regulation and mental wellness at risk.
Finding Your Balance
Mental wellness needs daily attention, much like physical therapy. These proven strategies help steady your mind:
Moving Within Your Limits:
- Gentle seated yoga
- Modified tai chi
- Breathing exercises
Caring for Your Mind:
- Quiet meditation moments
- Recovery journey journaling
- Achievable healing targets
Seeing recovery time as healing rather than waiting helps maintain optimism. This mindset shift transforms ‘rest’ from wasted time into productive healing.
Recognising When You Need Help
Sometimes professional support makes all the difference. Watch for these warning signs:
Key Changes to Notice:
- Ongoing feelings of loneliness
- Constant recovery worries
- Major sleep changes
- Lost interest in activities
Help comes in many forms. Video counselling sessions work well when movement proves difficult. Online groups connect you with others sharing similar challenges.
Reach out if you:
- Feel low for extended periods
- Worry constantly about recovery
- Notice eating pattern changes
- Feel cut off from others
Asking for help shows wisdom, not weakness. Healthcare providers understand how mental and physical healing work together. Adding mental health support to your recovery plan often leads to better results.
Daily Living Challenges
Simple daily tasks become complex puzzles when wearing a walking boot. Your usual routines, from work duties to personal care, need careful rethinking and adjustment.
How Will Work Life Change?
Office life takes on new challenges with a walking boot. Your usual workplace setup might need significant changes. Desk workers often discover their ergonomic arrangements no longer work, whilst active job roles require temporary adjustments.
Key workplace changes include:
- Desk adjustments for leg support
- Wheeled chairs for easier movement
- Work-from-home arrangements
- Standing desk modifications
What About Your Social Life?
Social gatherings feel different with a walking boot. The boot’s weight and bulk make simple social activities surprisingly challenging. Many patients find themselves turning down invitations, worried about mobility and comfort.
Common social hurdles include:
- Long periods of standing
- Moving through busy spaces
- Taking part in group activities
- Keeping up with regular plans
Can You Still Drive?
Driving deserves special attention when wearing a walking boot. Right-foot boots particularly affect your ability to control pedals safely.
Legal Points to Consider:
- No laws specifically ban boot driving, but vehicle control remains essential
- Insurance might not cover boot-related accidents
- The doctor’s approval might be needed
Safety Depends On:
- Which foot wears the boot
- Your car’s transmission type
- How well you can move
- Pain and medication effects
Public transport or lifts from others often prove safer options during recovery. Some doctors approve driving with specific boot adjustments, but this varies for each patient.
Keeping Clean and Fresh
Boot hygiene needs daily attention. Moisture trapped inside can lead to skin problems and unpleasant odours.
Daily Care Steps:
- Boot Cleaning:
- Remove washable parts
- Gentle wash with mild soap
- Complete drying before wearing
- Managing Moisture:
- Special moisture-control socks
- Regular sock changes
- Air breaks when resting
- Shower Safety:
- Waterproof boot covering
- Secure waterproof tape
- Safe shower seating
- Thorough drying after
- Fighting Odours:
- Regular cleaning routine
- Safe anti-bacterial products
- No oils or lotions nearby
Check any hygiene routine changes with your healthcare team, as some injuries need special care. Good boot maintenance keeps you comfortable and helps prevent problems during healing.
Conclusion
Walking boots protect injured ankles, yet their effects ripple through your entire body and daily life. Knowledge proves powerful – understanding these effects helps you face recovery challenges with confidence.
Your body faces significant changes. Most patients discover new pain points and notice their muscles weakening. Blood clots, especially DVT, demand vigilant attention and prevention. The way you walk shifts dramatically, threatening your posture and body alignment without proper care.
Life looks different with a boot. Sleep needs rethinking, work requires adjustments, and your mental health deserves extra attention. Strong support networks make these changes easier to handle. Regular talks with your healthcare team help address both body and mind throughout your healing journey.
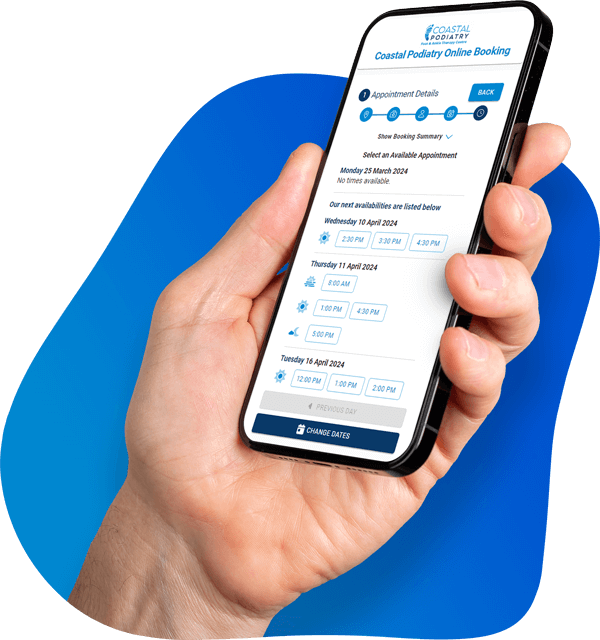
Concerned about the side effects of your walking boot? Coastal Podiatry’s experienced podiatrists can help you navigate your recovery and minimise complications. Contact us for advice and personalised treatment.
FAQs
What are the most common side effects of wearing a walking boot?
Common side effects include physical discomfort, changes in gait and posture, risk of blood clots, skin irritation, muscle weakness, and sleep disturbances. Many patients also experience mental health impacts due to limited mobility.
How long should I wear a walking boot each day?
Unless your doctor advises otherwise, you should wear the walking boot 24 hours a day, including at night. This ensures proper healing of your injury. However, the exact duration may vary based on your specific condition and your doctor’s recommendations.
Are there any activities I should avoid while wearing a walking boot?
You should avoid excessive walking, even if you’re allowed to bear weight. Don’t let your foot roll outwards when resting with the boot on. It’s important to follow your doctor’s instructions regarding weight-bearing and activity levels to prevent further injury.
What can I expect when transitioning out of a walking boot?
After removing the boot, your foot will likely feel weaker and more sensitive than usual. You should return to normal activities gradually, taking slow, easy steps at first. Supporting yourself when possible and following a rehabilitation plan can help strengthen your foot and ankle.
How can I manage hygiene issues while wearing a walking boot?
To maintain hygiene, clean the boot liner daily if removable, use moisture-wicking socks, and change them regularly. When showering, cover the boot with a plastic bag if it’s non-removable. Clean the boot regularly and use approved anti-bacterial products to prevent odours. Always consult your healthcare provider before modifying any care routines.